Overdoses Are Up, But Do We Really Need Just More Residential Beds?
By David Mee-Lee, M.D.
May 26, 2021
Editor’s Note: While this resource was initially published in 2021, the content around OUD and residential treatment is still a conversation being had today. The insights and questions asked in the below resource are still very real and relevant for us to consider today.
The Centers for Disease Control and Prevention (CDC) recently published a Vital Statistics Rapid Release document that showed overdose deaths during the pandemic rose to the highest levels since the opioid epidemic began:
- “at least 87,000 people died of a drug overdose in America” in the 12-month period ending last September, “an increase of 27% from the previous 12 months and a record for the most such deaths in a single year.”
- In that same period, “deaths attributed to synthetic opioids, mainly fentanyl, increased 53% nationwide.”
Tip 1
What do you believe should be the priorities for treatment of Opioid Use Disorder? Are more residential beds the answer?
With the overdose rates up, there is a push for more funding for addiction services. There should be, but often this is a call for more residential beds as if that is the first treatment of choice. Many still think of addiction treatment as:
- Sending the person “off to rehab”
- for some fixed length of stay (weeks or months) from which
- the person graduates, completes the program, and
- hopefully goes to Aftercare.
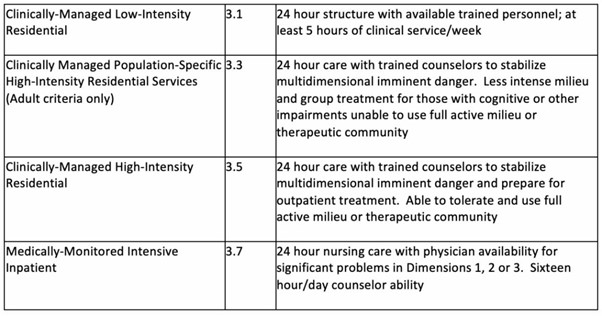
The ASAM Criteria (American Society of Addiction Medicine) articulates a continuum of care for addiction that includes but is not limited to residential treatment (See Table below).
Treatment Levels of Service (The ASAM Criteria 2013, pp 106-107)
- Outpatient Services
- Intensive Outpatient/Partial Hospitalization Services
- Residential/Inpatient Services
- Medically-Managed Intensive Inpatient Services
Tip 2
Some States have embraced longer lengths of stay in residential treatment as a priority in the opioid crisis. They limit Managed Care Organizations’ ability to require individualized treatment
Colette Croze, Principal of Croze Consulting asked me about residential levels of care and managed care authorization processes. Here, in part, is her question:
For the past five years I ….worked with many states as they developed their Centers for Medicare and Medicaid Services (CMS) 1115 Substance Use Disorders (SUD) waivers. Now I’m working with several on a variety of issues (residential utilization, expanding access to Medication for Opioid Use Disorder (MOUD), etc.)
A couple of the states are having difficulties with their Managed Care Organizations (MCOs) in terms of the length of authorization periods for residential treatment. I’m sure you’ve seen the tussle between MCOs who don’t really yet understand the purpose of residential treatment and providers who define it more often as a length of stay rather than a clinical regimen. While I totally embrace the principle that residential stays are individually based, it seems like there could be some “rules of thumb” as guidance for MCOs so that they’re not using the standard 3-day periods for initial and continuing authorizations. I’ve put some formative thoughts on paper and wondered if you’d be so kind as to give me feedback.
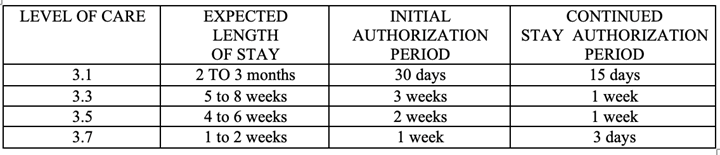
SUD RESIDENTIAL TREATMENT LEVELS OF CARE
EXPECTED LENGTH OF STAY, INITIAL AUTHORIZATION PERIOD AND CONTINUED STAY PERIOD
Reference Points from Other States
State #1 Medicaid Requirements of MCOs
- Level 3.1 No authorization for 90 days
- Level 3.5 No authorization for 14 days
- Level 3.7 No authorization for 14 days
State #2 Statute
- 2017 law: no authorization for 14 days
- 2020 revision: no authorization for 28 days
Proposal: Use these as benchmarks for recommendations on Medicaid requirements for MCOs around authorization periods, both initial and continued stay. (Also need to evaluate them in the context of the 1115 waiver cap of average residential use of 30 days/year.)
Tip 3
Recommending expected lengths of stay, and set authorization periods for initial and continued stay reviews works against individualized, outcomes-driven care.
Here is my response to Collette:
I understand the dilemma and your attempt to give some guidelines to MCOs. But such length of stay (LOS) guidelines perpetuate a program-driven, fixed LOS mentality. Two states, and maybe other states have instituted such LOS guidelines as a result, in my opinion of:
- Being concerned about the Opioid Crisis and that MCOs and money will drive people out of treatment.
- Being lobbied by residential treatment providers and a fixed LOS philosophy to give people more time in residential treatment free from “harassment” of MCOs.
- People (including legislators) are still not understanding that addiction treatment needs a continuum of care as in any chronic disease. Good outcomes require a long LOS in a continuum of addiction disease management, not a long LOS in “rehab” (residential).
- People are still focused on using residential treatment to do a ‘makeover’ of the person suffering from addiction in program-driven treatment for several weeks/months and then graduating.
What we need is:
- Not longer lengths of stay in residential, but more focus on using the full continuum of care.
- To move from program-driven care to person-centered, individualized treatment based on outcomes, not based on the program design, phases and “completion and graduation”.
- More community-based services to hang in with people for months and years just as we do for people with severe mental illness, not more residential beds and LOS.
- Assertive Community Treatment and Intensive Case Management teams to proactively engage and support people with severe, life-threatening addiction.
- More low barrier living supports (wet, damp and dry housing).
- More “Housing First” projects to engage people in treatment who are in Precontemplation about addiction treatment and recovery.
Unintended consequences
When there are recommended LOS guidelines and set authorization review periods:
- I see these turn into fixed ceiling LOS and programs keep clients for the maximum allowable days and then
- Providers apply for an allowable extension LOS because they are still focused on the program mentality.
- For example, if the initial allowable LOS is 30 days in residential with an allowable extension of 30 day increments up to 90 days, most clients stay 30 days and then get extensions for another one or two 30 day period.
- This keeps the field locked into a residential treatment mentality and not a chronic disease, continuum of care mentality.
Collette’s response:
Thanks for the thoughts. I couldn’t agree with you more about the over-reliance on residential treatment and the lack of patient-driven outpatient options. This current phase where providers and MCOs are lined up on different sides of the aisle is just so difficult.
This reprint of “Overdoses are up, but do we really need just more residential beds?” was written by David Mee-Lee, M.D. The original article may be accessed at https://tipsntopics.com/may-2021/.
Want to Read more?
To view this content, please sign up or log in to your account.
Create an account in seconds or log in if you’re already a member.
Sign Up
Sign In



